This post was originally published on this site
At least 65,000 more men died of COVID-19 in the U.S. than women in the period through August, and Black men are at higher risk than others, according to a new study published Wednesday.
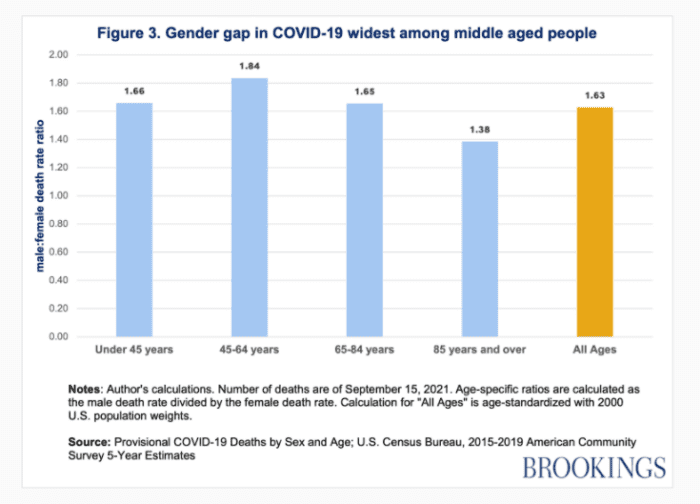
The study conducted by the Brookings Institution analyzed data from the Centers for Disease Control and Prevention and found the trend more pronounced among middle-aged men, with 184 male deaths for every 100 female deaths in that group.
“Notably, this gap does not appear to be explained either by differences in the number of confirmed cases or in pre-existing conditions,” the authors wrote.
The study’s main findings include: the overall death rate for men is 1.6 times higher than the rate for women; in Georgia and Michigan, Black men have the highest death rates, followed by Black women; and as death rates have fallen, the gender gap has eased slightly.
See also: U.S. life expectancy for people of color has plunged, primarily due to COVID-19
Source: Brookings Institution
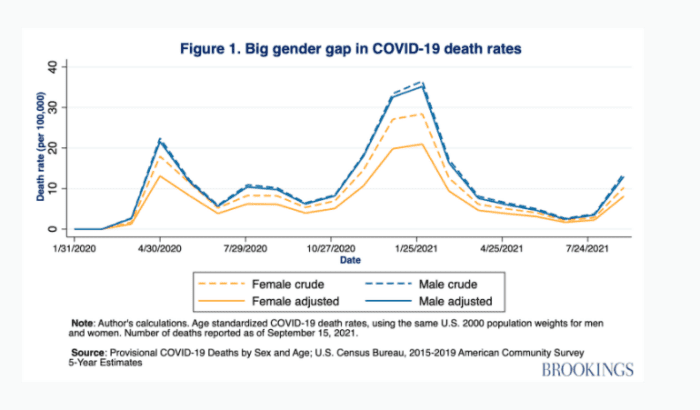
By the end of August, a total of 362,187 men had died of COVID, compared with 296,567 women. “The gender gap is even wider when differences in the male and female age distributions are taken into account, since there are many more older women than men in the population, and age is the biggest risk factor in COVID deaths,” the authors wrote.
Men aged between 45 and 64 saw almost twice the number of deaths as women in the same age group at 79,711 to 45,587. Men were 1.6 times more likely to die of the coronavirus-borne illness than women and men aged between 45 and 64 were 1.8 times more likely to die. The gap has narrowed since the start of mass vaccination, however.
Source: Brookings Institution
One reason for the gap could be that men are more likely than women to contract COVID in the first place, the CDC data shows. However, women account for slightly more cases, possibly because they also account for more of the high-risk jobs that expose them to COVID, such as healthcare, personal care and services and food preparation, the authors wrote. Those jobs are also likely to involve more testing, capturing mild and asymptomatic cases that are not always captured in men who are less likely to be tested for asymptomatic cases.
Race remains a key risk factor, the study found, in line with earlier findings that Black and Hispanic or Latino death rates are six times higher than for white people.
“This means that while there is a gap between men and women within racial groups, race is often a bigger factor,” the study found.
Read also:Since the start of the pandemic, 130 Black morticians have died in the U.S. from COVID-19
A study of data from Georgia and Michigan found the mortality rate for Black men was 170% times the rate for Black women, or significantly higher than the equivalent ratio among white people. The mortality rate for white men is 130% the rate for white women.
The authors are calling on policymakers to put renewed focus on immunizing the most vulnerable groups, which include men and especially Black men, who have lagged their white counterparts in getting their shots. White Americans are 6 percentage points more likely to have receive an initial dose of vaccine than Black Americans, at a rate of 41% to 35%.
“The racial disparity in vaccination rates is likely due to a combination of persistent barriers to access and structural inequities, which not only includes geographical access, but also logistics, methods of communication, timing, and registration,” the study found.
See now: WHO honors Henrietta Lacks, whose cells led to vast scientific breakthroughs

