This post was originally published on this site
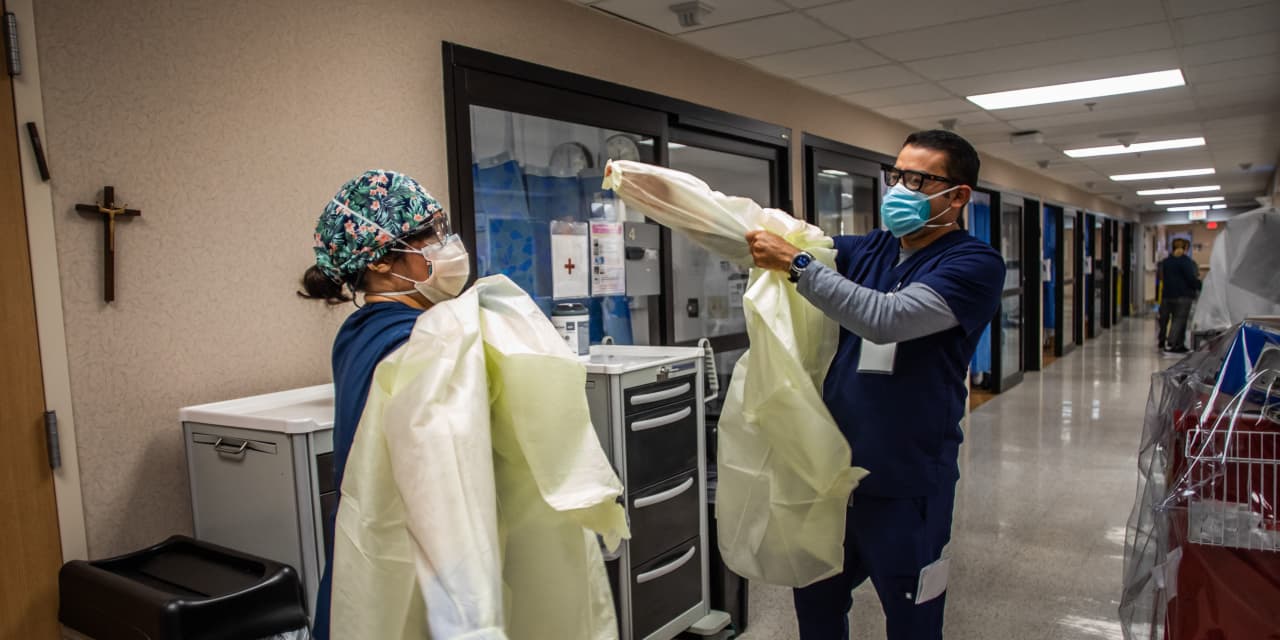
Hospitals are facing staffing shortages made worse by the COVID-19 pandemic, and Wall Street analysts are increasingly concerned that not having enough workers to staff these facilities will cut into margins.
“The rise in COVID-19 cases due to the delta variant continues to exacerbate the shortage of hospital workers, hampering recruitment and retention, driving up wages and weighing on hospitals’ profitability,” Moody’s Investors Service said Tuesday. “Over the next year, we expect margins to decline given wage inflation, use of expensive nursing agencies, increased recruitment and retention efforts, and expanded benefit packages that include more behavioral health services and offerings such as child care.”
There are several issues at play.
Nurses and doctors have been in short supply in some parts of the country for years. Many are burned out—and after 20 months of the pandemic, some are choosing to retire or quit. (A recent survey of 6,000 critical-care nurses found that 66% have considered quitting nursing because of the pandemic.)
“There’s no question the labor market has been pressured for some time, given the COVID activity,” William Rutherford, CFO of HCA Healthcare Inc.
HCA,
one of the largest hospital chains in the U.S., said last month at the Morgan Stanley Health Care Conference, according to a FactSet transcript of the presentation.
Then came the delta variant and a surge in hospitalizations that increased demand for nurses, in particular, to care for COVID-19 patients.
Many hospitals have had to limit or halt elective procedures considered key to their financial success to focus their resources on these patients.
This includes Intermountain Healthcare, Utah’s largest hospital system, which in mid-September began postponing all non-urgent procedures at 13 not-for-profit hospitals, citing a lack of beds. The same week, Idaho started allowing hospitals there to ration care, citing the “massive increase of COVID-19 patients requiring hospitalization in all areas of the state.”
“In some U.S. regions, hospitals have suspended elective overnight surgeries due not just to a rise in cases but also insufficient staffing, resulting in lost revenue,” Moody’s analysts wrote in the report.
And, finally, some workers have decided to quit or be fired rather than comply with COVID-19 vaccination mandates implemented by some health care organizations.
Add up all those factors, and then consider that salaries and benefits usually make up to half of a hospital’s total expenses.
Hospitals now have to pay workers more, including hiring more expensive temporary or travel nurses; spend more on benefits and other retention “perks”; and increase the amount of money they put into recruiting clinical talent. (This is a good thing for health care staffing firms like AMN Healthcare Services Inc.
AMN,
and Cross Country Healthcare Inc.
CCRN,
analysts say.)
“When COVID surges occur, hospital beds are allocated primarily to COVID patients and non-COVID admissions are being deferred,” Jefferies analysts wrote this week in a note to investors about not-for-profit hospitals. “As we exit the delta surge, we believe demand for temp nurses will temper from current levels but remain elevated (lower placement rates vs current averages) as deferred admissions and procedures are rescheduled.”
The delta surge is waning, and the number of new cases, hospitalizations, and deaths are declining. The current seven-day average for COVID-19 hospitalizations is 7,271, as of Friday, according to the Centers for Disease Control and Prevention. That’s already lower last week’s seven-day average of 8,378, but it doesn’t mean that all hospitals are out of the woods yet.
“Even as average daily COVID hospitalizations are decreasing, we continue to see many hospitals and intensive care units across the country at full capacity,” CDC director Rochelle Walensky said Wednesday during a White House briefing.
Read more of MarketWatch’s related coverage:



